Success Story
Improving the Prognosis of Patients with Leukemia
Clinical Trial
A novel drug-screening approach can help select treatment tailored to the individual patient
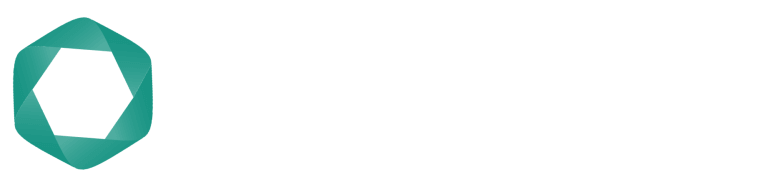
The PHRT Rapid-01 Trial is a randomized phase-2 clinical trial led by Berend Snijder of ETH Zurich. It will test whether an image-based drug screening approach called pharmacoscopy can improve the prognosis of patients with acute myeloid leukemia (AML). This rare form of blood cancer affects about 400 new patients in Switzerland every year. The disease leads to rapid proliferation of immature blood cells in the bone marrow and blood. Clinical symptoms include fatigue, easy bruising, and bleeding. It is the most common form of acute leukemia in adults, and if left untreated, AML is usually fatal within weeks or months. The current treatment is chemotherapy, sometimes in combination with a targeted therapy drug. However, not all patients respond. These patients, as well as those who suffer a relapse after standard treatment, generally have a poor prognosis.
"The feedback from the patients and the clinicians who are recruiting patients for the trial has been super positive."
Measuring how cells respond
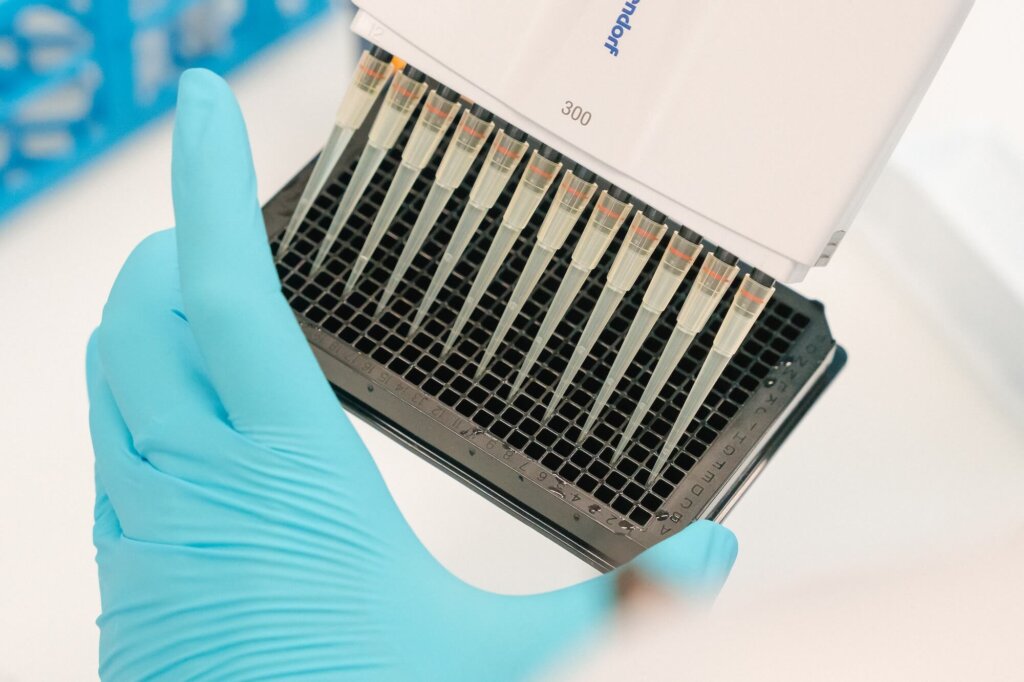
Over the past few years, systems biologist Berend Snijder has developed a screening platform that rapidly measures the cancer cells’ response to a large library of drugs. This might help select effective treatments tailored to the individual patient, thereby improving their prognosis. The technology works as follows: First, blood and bone marrow samples are taken from the patients and added to dishes with 384 wells. Each well contains a different drug that has been approved for AML. “We are currently testing 17 different drugs or combinations of drugs”, says Snijder. The dishes are then placed in an incubator and the cells interact with the drugs overnight. The next day, the cells are fixed and stained in order to distinguish healthy cells from cancer cells.
High-throughput automated microscopy is then used to take thousands of images per plate, resulting in images of millions of cells. “We can detect each single cell and evaluate each drug or drug combination: Did it kill the cancer cells, did it kill the healthy cells, did it kill all the cells?” A drug that kills both types of cells equally indicates general toxicity and is not a candidate of interest. “We’re looking for those drugs that specifically kill the cancer cells”, says Snijder. “The beauty of this approach is that it provides an internal control for toxicity.”
Pharmacoscopy-guided treatment requires only minimal sample volumes and helps inform the clinic in just a few days which treatment may be best suited for an individual patient. With an aggressive disease like AML, it is important to find an answer quickly.
Patient recruitment
In recent years, exploratory studies have shown that patients receiving pharmacoscopy-guided treatment have a higher event-free and overall survival compared to those receiving standard treatment. Now, in collaboration with Markus Manz and Alexandre Theocharides of the University Hospital Zurich, this approach will be evaluated in the world’s first randomized controlled phase-2 clinical trial for such a test. RAPID-01, as the trial is called, will enroll 88 patients with relapsed or refractory AML. Half of them will receive pharmacoscopy-guided treatment and the other half will receive standard treatment. The patients’ responses to the treatments will be assessed and compared after twelve weeks. “AML is an aggressive disease. If a treatment doesn’t work, it becomes clear very quickly”, says Snijder.
So far, 15 patients have been recruited. “The feedback from the patients and the clinicians who are recruiting patients for the trial has been super positive”, says Snijder. However, because eligibility criteria and regulations are strict, the recruitment process has been somewhat slower than expected.
To boost recruitment rates, the trial has been expanded to include patients from the Inselspital in Bern, and discussions are ongoing to also include the University Hospital Basel. The clinical trial expects to finish recruiting patients at the end of 2026. As the PHRT program officially terminates at the end of 2025, the scientists are relieved that they will be granted a cost-neutral extension until the end of 2026. This will allow them to answer the question of whether pharmacoscopy can help clinicians identify effective, patient-tailored treatments and improve the prognosis of patients with this deadly cancer.
In the meantime, pharmacoscopy-guided treatment is being extended to a wide range of other difficult-to-treat cancers. Preclinical trials have already been conducted in some other blood cancers as well as in glioblastoma, an aggressive form of brain cancer. “All of these studies look promising and further trials are underway. These are exciting times!”

Prof. Dr. Berend Snijder
ETH Zurich

Prof. Dr. Markus Manz
University Hospital Zurich

Prof. Dr. Alexandre Theocharides
University Hospital Zurich